Developing organs-on-chips to improve pregnancy outcomes
Pregnancy success as a result of in-vitro fertilisation (IVF) could improve due to research using organ-on-a-chip technology. Dr Virginia Pensabene is inserting real cells into a silicone chip in order to grow organs to investigate fertility problems.
Dr Virginia Pensabene is collaborating with scientists globally to further her research into growing organs-on-chips, with the aim of improving the efficacy of IVF procedures. Currently the success rate of IVF is as low as 30%.
Her patented new technology involves implanting and guiding real cells to grow in a miniature silicone chip. It has been thoroughly tested at the pre-clinical trial stage, which showed improvement of the IVF procedures in terms of cost saving and automation. The technology works by inserting the cell sample into the microfluid channels moulded into the silicone chip. The manufacturing process can produce organ models of different shapes and sizes by creating channels of different sizes.
...the pre-clinical trial stage...showed improvement of the IVF procedures in terms of cost saving and automation.
Dr Pensabene inserts isolated cells from a placenta into these channels. Then, hormones are used to guide the cells to behave as they would in the endometrium model – to replicate the menstrual cycle.
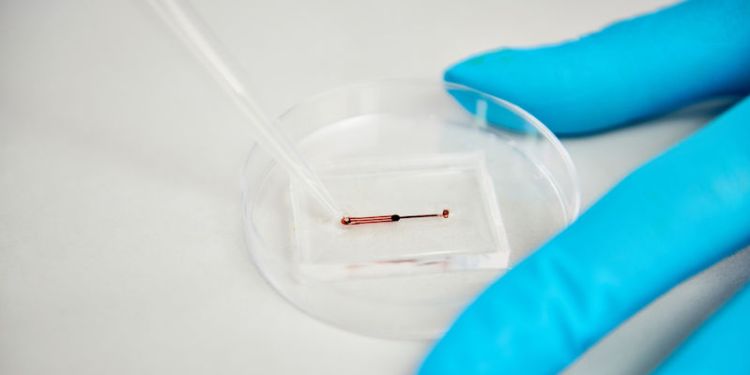
Isolated cells from a placenta are inserted into microfluid channels, then are guided by hormones to behave as they would in the endometrium model
The method examines how changes in different cell types mirror possible changes in the real organ to give insight into whether a particular treatment would work. Certain cells are more sensitive to mechanical stretching and to shear stress, such as the cells of the blood vasculature: if this stress is controlled, the cells will grow as they do in a real organ.
The next steps are to collaborate with key industrial partners to manufacture the device… with the research being able to move towards human clinical trials within the next three years.
The next steps are to collaborate with key industrial partners to manufacture the device. Patients and IVF experts who have helped to develop the project have contributed to the research being able to move towards human clinical trials within the next three years.

The manufacturing process can produce organ models of different shapes and sizes by creating channels of different sizes
Future solutions to fertility problems
Currently, the National Health Service (NHS) are only able to fund IVF treatment for one cycle, which has a failure rate of up to 98% of women aged 44 and above. As a result of this, financial and emotional stress is a risk for those undertaking the treatment.
Dr Pensabene and her team aim to improve implantation rates in IVF treatment and have already seen evidence of an improved in vitro embryo development (80% blastocysts rate) using murine and bovine embryos, which are the closest match to human embryos.
Investigating toxic exposure pregnancy risks
At the University of Leeds, Dr Pensabene aims to understand how the exposure to bacteria or toxicants in the environment can trigger adverse outcomes during pregnancy, such as miscarriage and premature birth. She will pursue this research using organ-on-chip models of the endometrium and the amniotic sac using human-derived cells.
Previously, Dr Pensabene worked with a leading team at Vanderbilt University that discovered that dioxin has detrimental effects on fertility that can be passed down to the next generation. Dioxin and other toxic chemical exposure can affect soldiers in warzones and cause fertility problems later.
Numerous everyday products, such as coffee cups, water bottles, and cosmetics, contain small amounts of harmful chemicals. The combination and accumulated quantity of these noxious materials can significantly affect our health.
Dr Pensabene is testing the effects of these toxins to examine how these factors can affect fertility and the reproductive system.

Benefits for students
Students and researchers at Leeds are able to apply the organ-on-chip method to a variety of different contexts due to the simplicity of the technology.
Projects delivered by students have included using a microfluidics system to examine progesterone and its links to the progression of Alzheimer’s.
Africa Smith de Diego, who is supervised by Professor Christoph Walti, is just one of the postgraduate researchers working with similar microfluidic systems in the bioelectronics lab.
Future development
University of Leeds, the Medical Research Council, and national organisations have funded Dr Pensabene’s research. She is now looking at translating this technology into a safe, cost effective, product for fertility treatments.
Dr Pensabene... is now looking at translating this technology into a safe, cost effective, product for fertility treatments.
The technique reduces the need for animals in lab testing as experimentation will take place in the chip, using human cells. Her findings could, in the future, aid policymakers with the potential to influence the use of chemicals linked to infertility, and other conditions such as cardiovascular disease and cancer.
Contact us
If you would like to discuss this area of research in more detail, please contact Dr Virginia Pensabene.
Related articles
Chips hold the key to reproductive health – IEEE Engineering in Medicine and Biology Society

